Symptoms of Sleep Apnea (7 Signs of Sleep Apnea)

Sleep apnea is a sleep disorder in which breathing repeatedly stops and starts during sleep. Although its most familiar symptom is snoring, not all those that snore have sleep apnea, and its effects on the body may wear out a person and leave them feeling exhausted during the day. If left untreated, it may have more severe health consequences. Knowing the signs of sleep apnea is the first step in understanding if you or a loved one may have it and when to seek medical intervention.
There are three types of sleep apnea: obstructive sleep apnea, central sleep apnea, and complex sleep apnea.
1. Obstructive sleep apnea
This type of sleep apnea, also known as obstructive sleep apnea-hypopnea, is the most common type of sleep apnea. It happens when the muscles in your throat recurrently collapse and cause a partial or complete blockage of airflow. Snoring is one of the most noticeable signs of obstructive sleep apnea because the person makes an effort to return to breathing when they stop.
Obstructive sleep apnea may be mild, moderate or severe, and the severity is usually measured with the apnea-hypopnea index (AHI). This measurement system counts the number of times a person’s breathing pauses, plus the periods of shallow breathing, that occur over an hour during sleep.
According to the American Academy of Sleep Medicine, mild obstructive sleep apnea means that a person has 5 to 15 episodes of breath pauses per hour. Moderate obstructive sleep apnea means that they experience 15 to 30 episodes per hour, and severe is anything above 30 events per hour.
People with abnormal jaw positions, obesity, nasal congestion, and large neck size are at an increased risk of experiencing obstructive sleep apnea.
2. Central sleep apnea
Central sleep apnea is a function of the central nervous system, and it happens when the brain doesn’t signal the body to keep breathing while you sleep. But it’s different from obstructive sleep apnea in the sense that people with central sleep apnea cannot try to breathe on their own when they notice they’ve stopped breathing because the brain and muscles are not functioning to that extent.
Snoring is also noticeable in central sleep apnea but is less evident compared to obstructive sleep apnea.
Central sleep apnea may be caused by conditions that affect areas of the brain responsible for controlling breathing, cervical spine injuries, stroke, heart attack, brain infection, heart failure, and surgery in the spine.
3. Complex sleep apnea
Complex sleep apnea occurs when a person has both obstructive sleep apnea and central sleep apnea.
When a person has sleep apnea, air stops flowing to their lungs, often for 10 seconds or longer—so they don’t breathe at all. In some people, this can happen over 30 times every hour. Sensing they have stopped breathing, a control center in the brain triggers them to wake up just enough to take a breath. Then they fall back to sleep, and the cycle begins again. They may not even remember waking up from this discomfort.
Sleep apnea remains a significant public health crisis as many people live with this disorder without any proper diagnosis. According to the American Academy of Sleep, about 80 to 90 percent of adults with obstructive sleep apnea remain undiagnosed.
A person with sleep apnea repeatedly wakes up and never really falls into the deeper and more restorative sleep stages. Also, the person’s heart rate and blood pressure continually rise in response to this event. As you can imagine, constantly being drawn out of and back into breathing, hour after hour, night after night, can strain the body.
Those with sleep apnea are more likely to fall asleep while driving. Several studies show that people with untreated sleep apnea have a significantly higher likelihood of being involved in a motor vehicle accident. Sleep apnea and chronic sleep deprivation can make it incredibly difficult to stay awake and stay focused on the road while driving. It may also slow down reaction time.
Additionally, according to a 2017 study published in the Journal of Neurosciences In Rural Practice, obstructive sleep apnea is associated with mental disorders like anxiety and depression and recommends that health professionals check their patients with obstructive sleep apnea for the disorder (specifically depression) to diagnose and treat them properly.
What are the symptoms of sleep apnea?
Many people with sleep apnea are unaware they wake up in between sleep cycles. All they know is they feel tired the next day.
A person’s bed partner usually observes the first and most common sign of sleep apnea: snoring. However, not all who snore have sleep apnea (although it is a common symptom). But with sleep apnea, snoring may be accompanied by gasping or choking sounds during sleep.
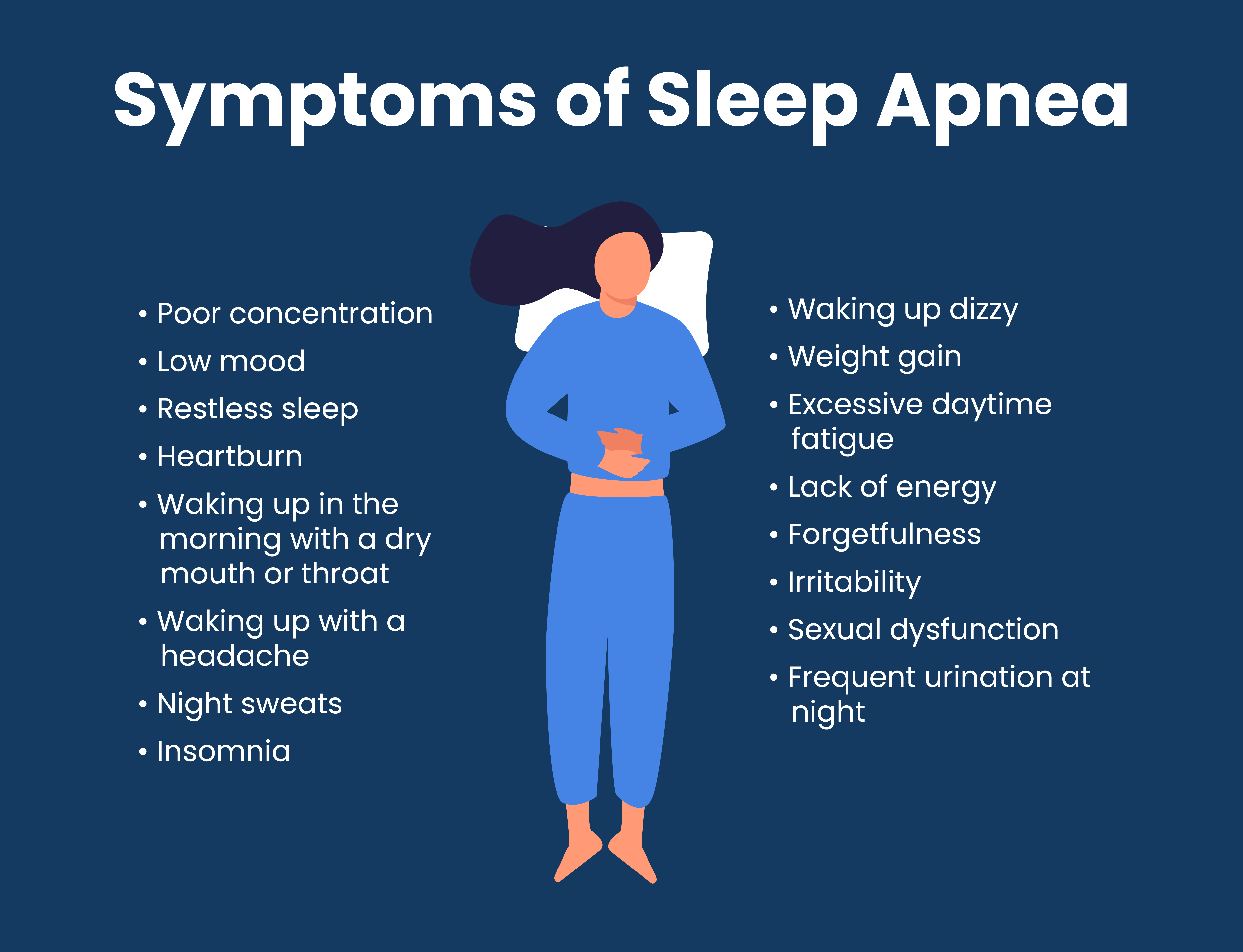
Some other sleep apnea symptoms are:
- Poor concentration
- Low mood
- Restless sleep
- Heartburn
- Waking up in the morning with a dry mouth or throat
- Waking up with a headache
- Night sweats
- Insomnia
- Waking up dizzy
- Weight gain
- Excessive daytime fatigue
- Lack of energy
- Forgetfulness
- Irritability
- Sexual dysfunction
- Frequent urination at night
These symptoms may not always relate to sleep apnea. However, discuss any concerns you may have with your doctor to get an accurate diagnosis and appropriate treatment.
Risk factors and consequences of sleep apnea
The risk for sleep apnea increases with age and with being overweight or obese. Although apnea affects both genders, men are at a higher risk of having it than women. People with a family history of snoring or sleep apnea may also be more prone to the disorder.
Bedtime alcohol consumption can also trigger sleep apnea. Generally, limiting alcohol intake (to two or less a day for men and one or less for women, daily by CDC’s recommendation) may help prevent this disorder.
Certain conditions like neurological disorders (Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), or Parkinson’s disease), hormonal disorders, post-menopausal symptoms, polycystic ovary syndrome, hypothyroid and hyperthyroid diseases, chronic kidney diseases, and chronic lung diseases are thought to be potential risk factors of sleep apnea.
Diagnosis requires a sleep study, either in your home or at a sleep lab. The most common treatment after diagnosis involves the use of continuous positive airway pressure (CPAP). Left untreated, however, sleep apnea can lead to severe consequences such as high blood pressure, heart disease, stroke, diabetes, and depression.
Seek medical guidance
If you think you might be experiencing sleep apnea, it’s best to talk to your doctor. If your doctor says that you’re not at risk for sleep apnea but that you snore more than you should, check out these snoring products tested and scored by sleep experts.
SleepScore Labs Solutions
The free SleepScore App tracks and measures your sleep, so you get an accurate depiction of what’s happening while you’re asleep. SleepScore’s patented sonar technology breaks down the time you spend in each sleep stage from light, deep, and REM sleep, along with the number of awakenings you have each night using just your smartphone.
If SleepScore notices atypical patterns that could suggest sleep apnea, you’ll receive a clinically validated screener to determine your risk level. From there, get connected with medical professionals to define the best next steps for your particular needs.
However, if you feel you need to see someone sooner rather than later, we always recommend connecting with your primary health care provider as soon as possible. Remember, a physician can make a diagnosis of sleep apnea following a clinical sleep study.