Don't sleep on your consumers' top unmet need - Better Sleep
Despite millions Googling ways to improve sleep, actionable guidance remains elusive. Over the last 20 years, sleep has become the most sought-after topic, surpassing even mental health, nutrition and fitness. SleepScore APIs offer a solution to this pressing need. Elevate your engagement and drive better health outcomes through hyper personalized sleep journeys and coaching - all grounded in the latest behavioral and circadian science and backed by studies & data.
Learn More About SleepScore APIs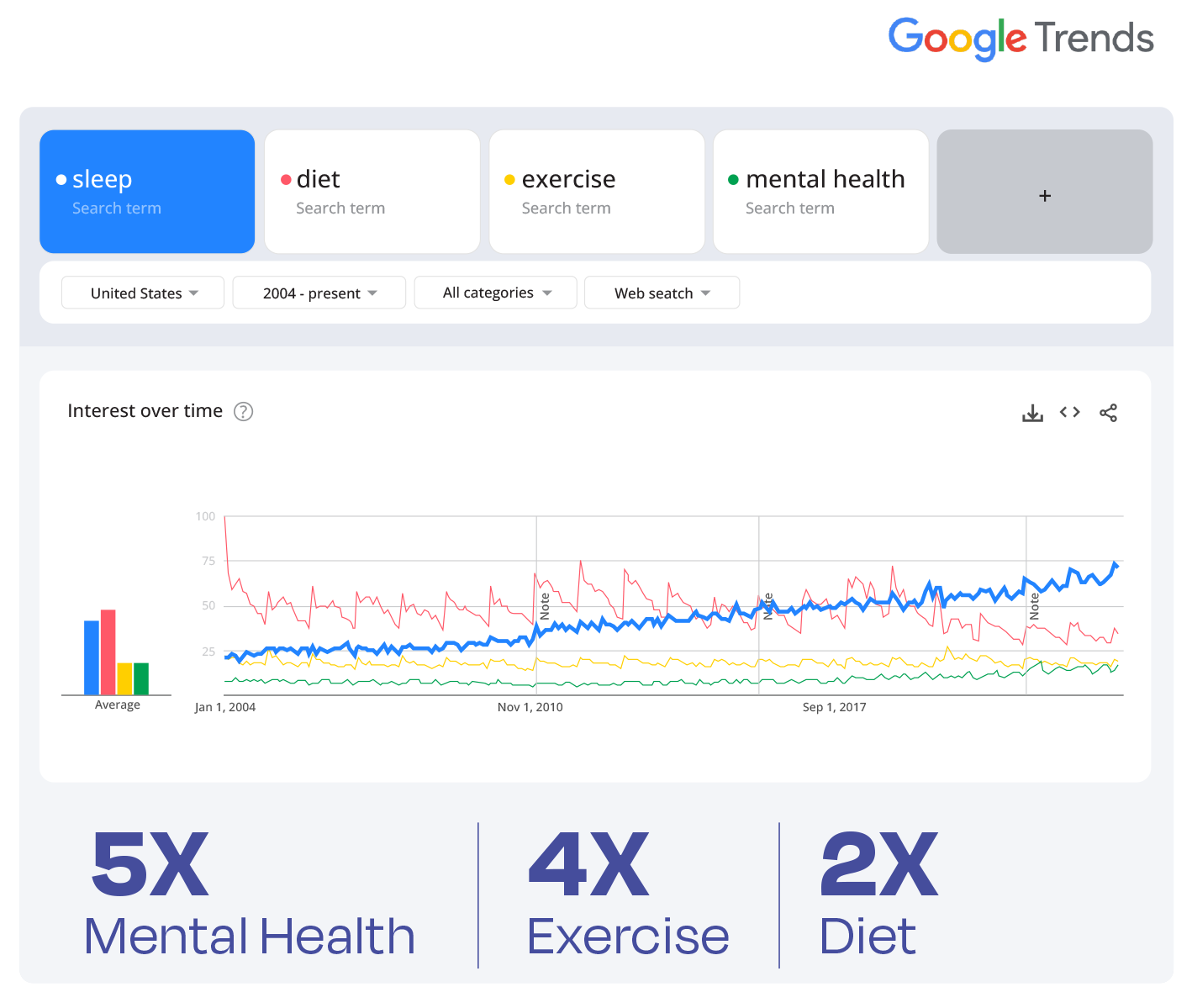
Trusted By












SleepScore APIs are pioneering the world's first (and still only) permanently reimbursed sleep improvement program for 74 million publicly insured people in Germany.
The only API's with 2 independent studies (one which is a randomized control trial) showcasing sleep improvement efficacy.
Proven results that supercharge growth
We're not just enhancing sleep outcomes; we're also driving engagement, bolstering retention, and optimizing health & wellness outcomes.
By utilizing user sleep data, including chronotype, behaviors, and motivations, we empower you to deliver better outcomes while simultaneously fueling your business growth.
Let's ConnectConsistent Engagement
3-4x
daily
Increased Retention
60-90%
after 30 days
More Exercise
up to 48%
increase in fitness activity
More Sleep
10-26
more hours of sleep per month*
* All objectively measured and statistically significant
Your consumers'
sleep is deeply personal
and we get that
That's why we're intentional about our robust data collection, analysis, and API delivery. Our APIs are precisely tailored to empower your consumers to confidently own their sleep journey through actionable lasting habits, constant learning, continuous improvement, and adaptive guidance.

SleepScore APIs - the forefront of sleep innovation
SleepScore APIs empower you to guide and inspire your consumers towards transformative sleep habits and outcomes. Backed by 360+ million hours of contextual sleep data, 61 peer reviewed publications and conference abstracts, and 230+ intervention studies. Get to know our APIs.
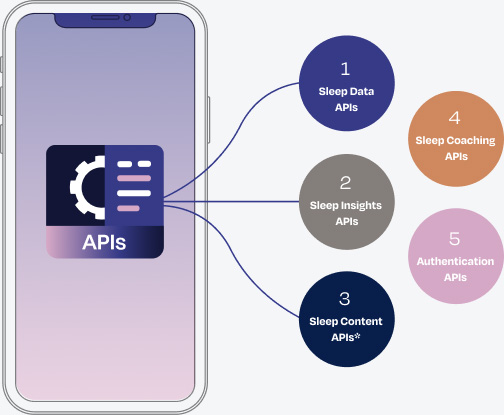
- Sleep Data APIs: Seamless collection of sleep data measured through wearables and apps
- Sleep Insights APIs: Actionable sleep insights tailored per phenotype - demographics, lifestyle, environment, and activity
- Sleep Content APIs: Thousands of engaging sleep and well-being related content material
- Sleep Coaching APIs: Personalized and adaptive sleep coaching rooted in science and Cognitive Behavioral Therapy (CBT)
- Authentication APIs: Secure connections across diverse systems and platforms
Sleep is the superhero inside health & wellness outcomes
While improving sleep may not always be your primary goal, it's the essential pathway to delivering on your health and wellness promise. Below are just a few data points showcasing the detrimental effect of poor sleep.
Weight Management / Loss:
Mental health:
Fitness / Athletics:
Women's Health:
Longevity:
A partner you won't lose any sleep over
Science & data experts
across our team, advisory board, and academic partners we have solid scientific evidence in real-world settings
Trusted across industries
to set the standard for sleep performance across industries, revolutionizing sleep wellness
Device & data agnostic
collecting, analyzing, and acting on the data you trust with hundreds of devices and apps already supported
Deliver seamless integration
of sleep data, insights, coaching, content, and authentication APIs into your tech infrastructure, & journeys
Unwavering commitment
so you can rely on our team for support and guidance every step of the way
Spun out of & backed by ResMed
the global leader in sleep medical devices, with a legacy of expertise & innovation, setting us apart as your partner
Seize the Zzz's with SleepScore APIs
Change your consumers' relationship with sleep and enable them with evidence-based health & wellness outcomes.
Explore SleepScore APIs nowSources
- Nedeltcheva, A. V., Kilkus, J. M., Imperial, J., Schoeller, D. A., & Penev, P. D. (2010). Insufficient sleep undermines dietary efforts to reduce adiposity. Annals of internal medicine, 153(7), 435-441.
- Taheri, S., Lin, L., Austin, D., Young, T., & Mignot, E. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS medicine, 1(3).
- Blackwelder, A., Hoskins, M., & Huber, L. (2021). Effect of Inadequate Sleep on Frequent Mental Distress. In Preventing Chronic Disease (Vol. 18). Centers for Disease Control and Prevention (CDC).
- Nutt, D., Wilson, S., & Paterson, L. (2008). Sleep disorders as core symptoms of depression. Dialogues in clinical neuroscience, 10(3), 329-336.
- Azboy, O., & Kaygisiz, Z. (2009). Effects of sleep deprivation on cardiorespiratory functions of the runners and volleyball players during rest and exercise. Acta Physiologica Hungarica, 96(1), 29-36.
- von Rosen, P., Frohm, A., Kottorp, A., Fridén, C., & Heijne, A. (2017). Multiple factors explain injury risk in adolescent elite athletes: applying a biopsychosocial perspective. Scandinavian journal of medicine & science in sports, 27(12), 2059-2069.
- Mah CD, Mah KE, Kezirian EJ, Dement WC. The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep. 2011 Jul 1;34(7):943-50
- Latiri, I., & Dogui, M. (2016). Effects of one-night sleep deprivation on selective attention and isometric force in adolescent karate athletes. The Journal of Sports Medicine and Physical Fitness, 57(6), 752-759.
- Nam, G. E., Han, K., & Lee, G. (2017). Association between sleep duration and menstrual cycle irregularity in Korean female adolescents. Sleep medicine, 35, 62-66.
- Samaraweera, Y., & Abeysena, C. (2010). Maternal sleep deprivation, sedentary lifestyle and cooking smoke: Risk factors for miscarriage: A case control study. Australian and New Zealand Journal of Obstetrics and Gynaecology, 50(4), 352-357.
- Ahlborg Jr, G., AXELSSON, G., & Bodin, L. (1996). Shift work, nitrous oxide exposure and subfertility among Swedish midwives. International journal of epidemiology, 25(4), 783-790.
- Hublin, C., Partinen, M., Koskenvuo, M., & Kaprio, J. (2007). Sleep and mortality: a population-based 22-year follow-up study. Sleep, 30(10), 1245-1253.
- Daghlas, I., Dashti, H. S., Lane, J., Aragam, K. G., Rutter, M. K., Saxena, R., & Vetter, C. (2019). Sleep duration and myocardial infarction. Journal of the American College of Cardiology, 74(10), 1304-1314.
- Sabia, S., Fayosse, A., Dumurgier, J., van Hees, V. T., Paquet, C., Sommerlad, A., ... & Singh-Manoux, A. (2021). Association of sleep duration in middle and old age with incidence of dementia. Nature Communications, 12(1), 2289.
- Gottlieb, E., Egorova, N., Khlif, M. S., Khan, W., Werden, E., Pase, M. P., ... & Brodtmann, A. (2020). Regional neurodegeneration correlates with sleep-wake dysfunction after stroke. Sleep, 43(9).
- Spiegel, K., Tasali, E., Leproult, R., & Van Cauter, E. (2009). Effects of poor and short sleep on glucose metabolism and obesity risk. Nature Reviews Endocrinology, 5(5), 253-261.
- Kim, M. A., Kim, E. J., Kang, B. BY., & Lee, H. K. (2017). The effects of sleep deprivation on the biophysical properties of facial skin. Journal of Cosmetics, Dermatological Sciences and Applications, 7(1), 34-47.



